2 years ago · hillside · 0 comments
The Causes, Symptoms, and Diagnosis of Epilepsy?
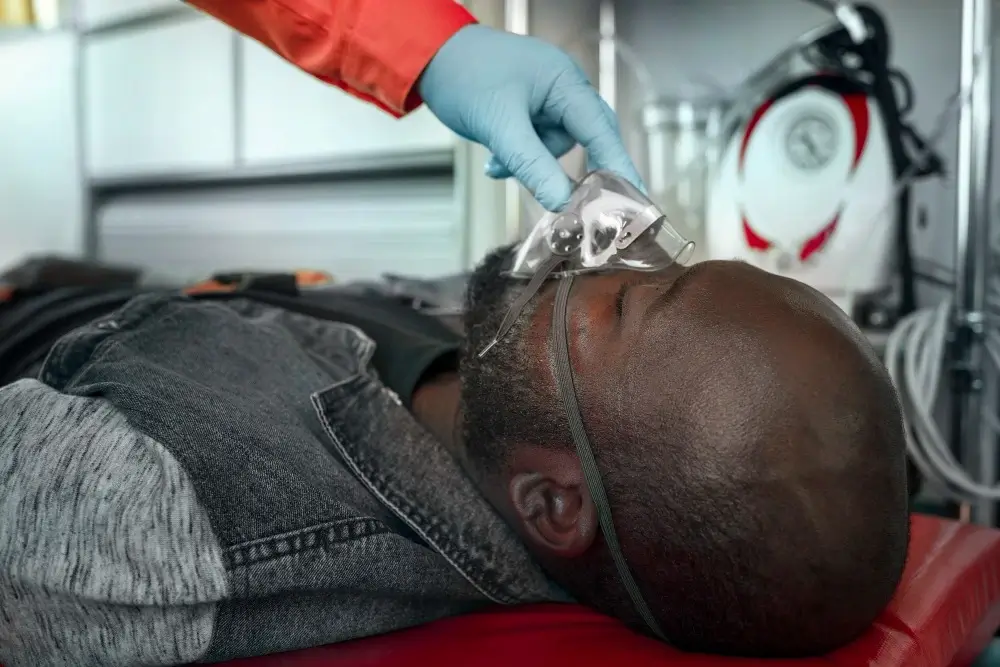
Join us on a journey to demystify epilepsy. We’ll break down the complexities step by step, aiming to provide a clear understanding of this neurological condition and its various facets. We Will explore the causes, symptoms, and diagnosis of epilepsy, making this intricate topic accessible to all. Together, let’s navigate through the essential aspects of epilepsy, shedding light on its origins, signs, and diagnostic procedures.
What does “Epilepsy” mean to you?
Epilepsy is a chronic neurological disorder characterized by recurrent, unprovoked seizures. Seizures are sudden, abnormal bursts of electrical activity in the brain, which can lead to a wide range of symptoms and behaviors, from brief lapses in consciousness or subtle sensory changes to more severe convulsions and loss of motor control. Epilepsy can affect people of all ages and can be caused by various factors, including genetic predisposition, brain injuries, infections, or underlying medical conditions. Accurate diagnosis and appropriate treatment are essential in managing epilepsy and improving the quality of life for individuals with the condition.
The 10 Common Underlying Causes of Epilepsy.
Welcome to our exploration of the underlying causes of epilepsy, we will embark on a journey to unravel the mysteries surrounding this neurological condition. By delving into these essential factors, we aim to provide a clear and accessible understanding of what contributes to epilepsy. Join us as we navigate through the core aspects that shed light on the origins of this condition.
- Brain Abnormalities. Structural issues in the brain, such as tumors, malformations, or scar tissue from head injuries, can disrupt normal brain function, leading to epilepsy. These abnormalities may interfere with the brain’s electrical activity, causing seizures. A classic example is someone developing epilepsy after a traumatic brain injury in a car accident.

- Genetic Factors. Epilepsy has a genetic component, which means that if you have family members with epilepsy, your risk may be higher. Certain genes, like SCN1A, can increase susceptibility. A clear understanding of the genetic underpinnings is essential for diagnosis and tailored treatment. For instance, Dravet Syndrome, a severe form of epilepsy, is often associated with specific genetic mutations.
- Head Injuries. Head injuries, even seemingly minor ones like concussions, can trigger epilepsy. Athletes involved in contact sports are at risk due to repetitive head trauma. Understanding the relationship between head injuries and epilepsy is crucial, as early detection can help prevent or manage the condition.
- Infections. Infections that affect the brain, such as meningitis or encephalitis, can lead to epilepsy. One notable example is the herpes simplex virus, which can cause viral encephalitis. Identifying and treating infections promptly is essential to reduce the risk of epilepsy.
- Developmental Disorders. Certain developmental disorders like autism and neurofibromatosis are associated with an increased risk of epilepsy. It’s important to recognize the coexistence of these conditions and their shared neurological factors. This understanding can aid in early intervention and treatment strategies.
- Febrile Seizures. Febrile seizures are often associated with children who experience high fever. While not all children who have febrile seizures develop epilepsy, it is a potential risk factor to be aware of. Timely medical attention and fever management can reduce the likelihood of epilepsy in these cases.
- Brain Tumors. Brain tumors, whether benign or malignant, can exert pressure on the brain and disrupt its normal function. This pressure can lead to seizures. A glioma in the temporal lobe, for example, can cause seizures, emphasizing the importance of early tumor detection and intervention.

- Metabolic Causes. Metabolic imbalances, like hypoglycemia (low blood sugar) or electrolyte imbalances, can provoke seizures. Diabetic individuals who experience severe hypoglycemia may be at risk of developing epilepsy. Maintaining stable metabolic health is crucial in preventing these seizures.
- Strokes. Strokes can damage the brain’s blood vessels, resulting in inadequate oxygen supply to brain cells. This deprivation can trigger seizures. Ischemic strokes, caused by blood clots, are a common cause of epilepsy, highlighting the necessity of stroke prevention and timely treatment.
- Environmental Factors. Environmental factors like lead poisoning or exposure to toxins can increase the risk of epilepsy. Lead exposure in children, for instance, can lead to neurological damage and seizures. Identifying and eliminating these environmental hazards is critical to preventing epilepsy associated with them.
The 8 Common Symptoms You Should Know About.
It’s essential to be aware of the symptoms of epilepsy, as early recognition can lead to timely diagnosis and appropriate care. We will explore eight common epilepsy symptoms in a clear and straightforward manner, helping you understand this condition better.
- Seizures. Epileptic seizures are the hallmark of this condition. They manifest in diverse ways, from subtle momentary lapses in awareness to more dramatic convulsions. Seizures occur due to abnormal electrical activity in the brain, causing sudden, uncontrolled bursts of movement or sensations.
- Loss of Awareness. During seizures, individuals may suddenly lose awareness and become unresponsive. This disorienting phase is known as the ictal state, and it can be followed by confusion. Sufferers often have no recollection of the episode.

- Repetitive Movements. Some seizures involve repetitive and involuntary movements, such as lip-smacking, clothing-picking, or hand-wringing. These behaviors can be a telltale sign of an ongoing seizure.
- Sensory Changes. Epileptic seizures can provoke unusual sensory experiences. People may report odd tastes, smells, or visual distortions. These sensory disturbances can provide important clues for diagnosis.
- Muscle Stiffness. A common symptom is muscle stiffness or rigidity, which can make it hard to move during a seizure. It may cause a person to fall or result in an uncomfortable physical sensation.
- Emotional Changes. Some individuals experience intense emotional changes before or after seizures. These can include fear, anxiety, or a sense of déjà vu. These emotional shifts can be as disconcerting as the physical symptoms.
- Involuntary Urination. Epileptic seizures can lead to the loss of bladder or bowel control, which can be distressing for those affected. Understanding this aspect is crucial for caregivers and loved ones.
- Recovery Period. After a seizure, there is a postictal state where individuals may feel confused, exhausted, or even experience a headache. This phase is part of the seizure event and may vary in duration. Recognizing and assisting during this period is vital for the person’s well-being.
The Diagnosis of Epilepsy 7 Key Steps to Understanding.
Epilepsy, a neurological disorder characterized by recurrent seizures, affects millions worldwide. The path to an accurate diagnosis can be complex, involving various essential steps. Let’s explore the seven key components of epilepsy diagnosis, making it easy to grasp for all readers.
- Clinical Evaluation for Epilepsy.
The journey begins with a thorough clinical evaluation by a healthcare professional. This process includes discussions about the patient’s medical history, an in-depth review of symptoms, and observations of seizure characteristics. It is the foundation of the diagnosis.
- Diagnostic Tests for Epilepsy.
Diagnostic tests are crucial in confirming epilepsy. The electroencephalogram (EEG) is one of the primary tools used to record and analyze brain wave patterns, identifying any abnormal electrical activity that may be associated with seizures.
- Neuroimaging in Epilepsy Diagnosis.
Neuroimaging techniques such as magnetic resonance imaging (MRI) and computed tomography (CT) scans help identify structural abnormalities in the brain, including tumors, lesions, or scarring, which could be the root cause of seizures.

- Seizure Monitoring in Diagnosis.
Sometimes, long-term monitoring is necessary. Video EEG monitoring in a hospital setting allows medical professionals to observe and record seizures as they happen, ensuring a more precise diagnosis.
- Differential Diagnosis of Epilepsy.
Differential diagnosis is the process of distinguishing epilepsy from other conditions that may resemble it, like syncope (fainting) or psychogenic non-epileptic seizures (PNES). This step ensures that the correct diagnosis is made.
- Advanced Diagnostics in Epilepsy.
Neuropsychological testing is often employed to assess cognitive functions and potential behavioral changes associated with epilepsy. These tests provide valuable insights into the impact of seizures on an individual’s daily life.
- Diagnostic Accuracy in Epilepsy.
The accuracy of the diagnosis is of utmost importance. Healthcare providers use a combination of clinical evaluation, diagnostic tests, and medical history to ensure that epilepsy is correctly identified, enabling the development of a suitable treatment plan.
Conclusively, a comprehensive understanding of epilepsy, its causes, symptoms, and diagnostic procedures is crucial for timely care. Recognition of common symptoms and accurate diagnosis through clinical evaluation and advanced tests ensures proper support and reduces stigma, fostering awareness and appropriate care for individuals with epilepsy.
By: Mugambwa Methodius.

Leave a Reply